Pleural Effusion: Exudative vs Transudative
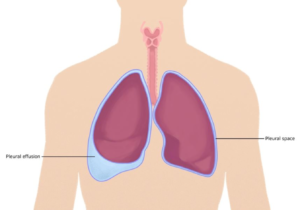
Pleural effusion is the abnormal collection of fluid in the pleural space. The pleural space normally contains 10 ml of fluid for lubrication. Pleural effusion can be categorized into parapneumonic, empyema, hemothorax, and chylothorax based on their pathophysiological processes. Pleural effusion can also be classified based on possible etiologies into transudative and exudative.
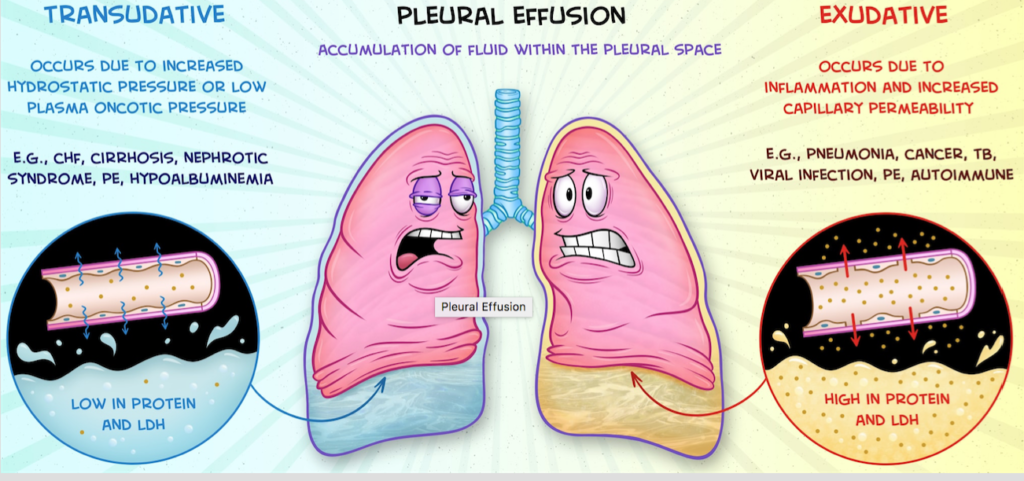
Transudative effusionsare caused by systemic diseases that result in an increased hydrostatic pressure (pressure that forces fluid out of capillaries) or a decreased oncotic pressure (pressure that draws fluid back into the capillaries). Increased hydrostatic pressure can occur during heart failure in which the heart cannot pump efficiently leading to back up of blood into the lungs and to an increase in the pulmonary blood pressure. The high blood pressure pushes fluid out of the capillaries into the pleural space causing pleural effusion. Decreased oncotic pressure can happen in cirrhosis and nephrotic syndrome in which protein (albumin) production decreases or it is lost in the urine, respectively. Due to decreased oncotic pressure, fluid leaks out of the capillary into the pleural space causing pleural effusion.
Exudative effusionsresult from local diseases that cause inflammation of the lung capillaries. Inflammation makes capillary more permeable allowing fluid, immune cells and large proteins (like LDH) to diffuse out of capillaries into the pleural space. Aside from capillary inflammation, exudative effusion can occur from impaired lymphatic drainage of the pleural space. Causes of exudative effusion include trauma, malignancy, and inflammatory diseases like lupus or pneumonia.
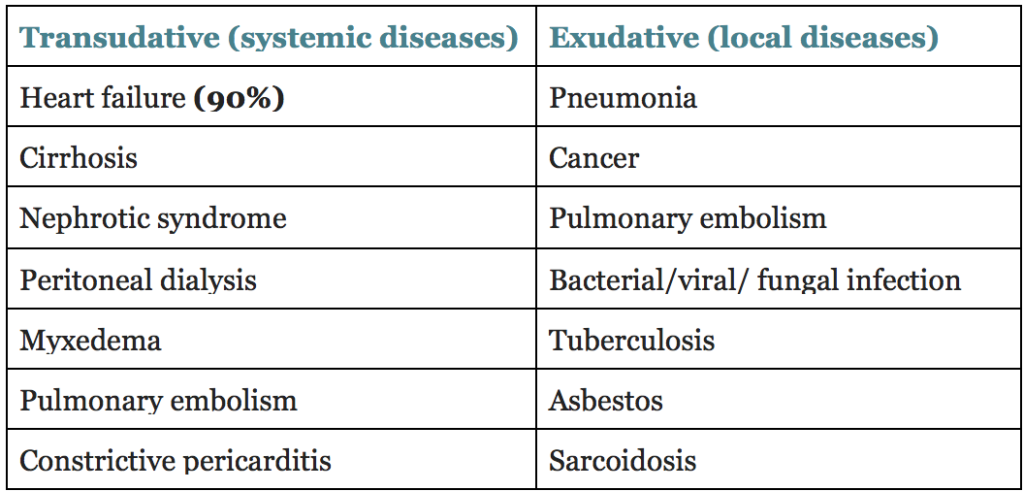
Causes of transudative and exudative effusion
Signs and Symptoms Generally, patients report dyspnea, cough or pleuritic chest pain. Large effusions are more likely to cause symptoms than a small effusion. Physical exam findings include dullness to percussion, decreased fremitus, and decreased breath sounds. Patients might have pleural friction rub. A massive effusion can cause contralateral shift of the trachea and protrusion of the intercostal spaces.
Diagnosis Chest x-rayis the initial test of choice. A lateral decubitus and PA views are usually obtained. The lateral decubitus position helps to determine if the effusion is an empyema, loculation or a small effusion. Presence of a meniscus signor blunting of costophrenic angle is indicative of pleural effusion.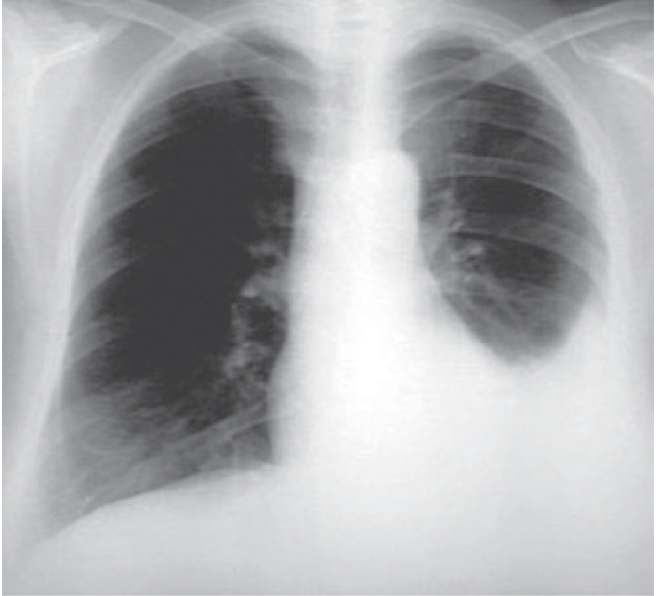 Left pleural effusion
Left pleural effusion
Thoracentesis is the gold standard. It can be used for diagnostic and therapeutic purposes. It helps to distinguish between a transudative and exudative effusion. When fluid is collected, it is analyzed for protein, glucose, LDH and WBC. Transudative has less protein, and it is clear in appearance. Exudative has much more proteins, and it is cloudy in appearance due to the presence of immune cells. However, to accurately differentiate between these two types of effusions, the Light criteria is used to determine the presence of exudative effusion. An exudate is present if at least one of these 3 criteria are met:
- Pleural fluid protein: serum protein >0.5 or
- Pleural fluid LDH: serum LDH >0.6 or
- Pleural fluid LDH > ⅔ the upper limit of normal LDH.
Treatment
- The mainstay treatment is to treat the underlying cause.
- Observation is an adequate approach in some situations such as effusion caused by heart failure.
- Thoracentesis can be diagnostic and therapeutic.
- Chest tube fluid drainage in cases of empyema
- Pleurodesis (causing the pleural layers to stick together) in cases of malignancy or chronic effusion with talc, doxycycline or minocycline.
Peds online case In the hospital, the pleural fluid of the patient was analyzed. Results: yellow, cloudy, RBC 18k, 100 WBC (37 neutrophil), glucose 69, fluid LDH 327, serum LDH 224, serum protein 5.3 and fluid protein 3.4.
Pleural fluid protein: serum protein →3.4 / 5.3 →0.64
Pleural fluid LDH: serum LDH →327/ 224 →1.45
Pleural fluid LDH > ⅔ the upper limit of normal LDH
In this case, the pleural effusion is exudative. At least one of the light criteria was met. In addition, the fluid was yellow and cloudy.
Sources
- Chesnutt, Asha N., et al.. “Pleural Effusion.” Current Medical Diagnosis and Treatment 2020 Maxine A. Papadakis, et al.New York, NY: McGraw-Hill, , http://accessmedicine.mhmedical.com.york.ezproxy.cuny.edu/content.aspx?bookid=2683§ionid=225058693
- https://www.osmosis.org/learn/Clinical_Reasoning:_Pleural_effusion?playlist=clinicalreasoning
- https://www-uptodate-com.york.ezproxy.cuny.edu/contents/diagnostic-evaluation-of-a-pleural-effusion-in-adults-initial-testing?search=pleural%20effusion&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1#H6
- https://www.osmosis.org/learn/Pleural_effusion
- Pance Prep Pearls. Page 142