Daniela Arias Rodriguez
Pediatric H&P#2 1/5/21
Identifying Data:
Name: RP
Date of Birth: 17 yrs old
Gender: Male
Date & Time: January 5, 2021
Location: Queen Hospital Center
Source of Information: self and mother
Chief complaint:Epigastric abdominal pain and vomiting x 3 days
DDX:
Cholecystitis
Cholangitis
Choledocholithiasis
pancreatitis
Hepatitis A or B
Gastritis
GERD
Viral enterocolitis
Bacterial enterocolitis
pneumonia
HPI: RP is a 17 y/o male without Pmhx who was brought to the ED by ambulance (accompanied by mother) with complaints of epigastric pain and vomiting x 3 days. Pt reported that abdominal pain started gradually two days prior in the upper abdomen followed by a non-bloody vomitus after having lunch. He describes the epigastric pain as dull, intermittent, non-radiating, and 10/10 without any alleviating or worsening factors. In the past 3 days, pt has vomited around ten times and admits decreased fluid and food-intake. He also reports feeling weak and fatigue and admits yellowish discoloration in eyes. Pt presented previously to the ED on 1/3/21 with the same complaints and was discharged with a diagnosis of gastritis and prescribed famotidine. Pt reports being compliant with the prescribed medication without any relief. Pt denies taking any other medication at home. Today, pt denies fever, diarrhea, bloody stools, constipation, chill, eating anything abnormal, chest pain, productive cough, recent travel, alcohol use, sick contact or positive COVID contact.
Past Medical History:
Present illnesses – none
Past illness- none
Hospitalized – none
Immunizations – not up to date with all vaccines
Past Surgical History: none
Medications: Famotidine 20mg bid for 2 days.
Allergies: Denies
Family History: non-contributory
Social History:Domiciled with mother and currently attending high school. Pt came from Guyana six years ago. Pt is not sexually active and denies hx of STDs. Pt denies use of alcohol, drugs or smoking.
ROS:
Gen –Admitsdecreased appetite,fatigue and weakness.Denies weight loss, fever, chills or night sweats.
Skin, hair, nails—Denies hair loss, excessive sweating, dryness, or skin change texture.
Head— Denies head trauma, dizziness and headache.
Eyes— admits yellowing of the eyes. Denies blurring vision, dryness, lacrimation or fatigue.
Ears— Denies ear pain, discharge, hearing difficulty or tinnitus.
Nose/sinuses—Denies nose bleed, discharge or obstruction.
Mouth/throat—Denies sore throat, bleeding gums, mouth ulcers or changes in voice.
Neck—Denies swelling, lumps or decreased range of motion
Pulmonary – Denies SOB, cough, hemoptysis or wheezing.
CV—Denies chest pain, peripheral edema, palpitation or known heart murmur.
GI— Admits epigastric pain, vomiting x 3 days and jaundice.Denies hemorrhoids, dysphagia, jaundice, diarrhea or constipation.
GU—Denies hematuria, frequency, urgency, or dysuria.
Nervous— AOx3. Denies numbness, tingling, headaches or hx of seizures.
Musculoskeletal— Admits weaknessand denies swelling or muscle/joint pain.
Hematological— Denies easy bruising, anemia, hx of blood transfusion or DVT/PE.
Endocrine—Denies polyuria, diaphoresis, polydipsia, heat or cold intolerance
Psychiatric— Denies depression, suicidal ideations or thoughts.
1/5/21
VS:T: 98.3 F, HR 78 bpm, BP 120/70 right arm lying, RR 18, SpO2 100% room air, BMI: 26.0
Physical Exam:
Gen– AOx3, small build, lying in bed in visible distress and discomfort.
Skin: mildly icteric, warm, non-diaphoretic, capillary refill <2 second.
Head:Normocephalic, atraumatic with no tenderness to palpation.
Eyes: icteric and pale conjunctiva bilaterally. PERRLA, full visual fields and intact EOM with no nystagmus.
Ears: intact tympanic membrane. Auditory canal without erythema or discharge bilaterally.
Mouth: Pink and moist mucosa no masses or tonsil exudate noted. Uvula middle line. Good dentition.
Lungs: Clear to auscultation bilaterally. No rales, rhonchi or wheezing on auscultation.
Cardiac:Normal S1/S2 and RRR. No murmur, JVD or carotid bruits.
Abdomen: Soft, flat abdomen, + bowel sound in all quadrants. Generalized tenderness with prominence in the epigastric area. Negative murphy sign, psoas, and obturator. No rebound tenderness or guarding.
Rectal: Denies
Extremities: Full active ROM in upper extremities bilaterally. 2+ pulses in upper and lower extremities. No sign of edema.
Labs
Anion gap 14
Chloride 100 Creatinine 0.97
Na 137 C02 23 glucose 196
K 4.2 BUN 16 Lipase 26
ALT >7000 Total. B 6.2
AST >4,781 Direct. B 1.1
ALK 135
CBC
WBC: 9.75 MCV 83.8 PLT 156
RBC: 5.67 MCHC 34.1 Neutrophil 82.8
Hgb: 16.2 Lymphocytes 7.1
Hct: 47.5 RDW 12.8
PTT 31.3 Hep A Ab IgM: indeterminate
INR 3.0 Hep B surface Ag: non-reactive
PT 35.1 Hep B core IgM antibody: non-reactive
Hep C: non-reactive
Acetaminophen toxicity <5
Assessment/plan:RP is a 17 y/o male without Pmhx presented to the ED with severe epigastric pain and multiple vomiting episodes. Physical exam was significant for jaundice and elevated liver enzymes. Pt was given IV bolus, IV Zofran and transferred to Cohen Children’s Medical Center for further work-up. After several days, Hep A came back as indeterminate.
Article Summary
Gastrointestinal Symptoms and Elevation in Liver Enzymes in COVID-19Infection: A Systematic Review and Meta-Analysis. Puli S, Baig M, Walayat S.Cureus. 2020 Aug 24;12(8):e9999. doi:10.7759/cureus.9999. PMID: 32983698 Free PMC article.
- This is a systematic review and meta-analysis published in August 2020. Journal is not currently indexed by Medline. It included a total of 15 articles with a total sample size of 3762 of which 404 patients had a severe COVID-19 infection.
- This study aimed to analyze the GI manifestations and elevated liver enzymes in patients diagnosed with COVID-19.
- Of the included studies, 13 were conducted in China, 1 in the United states and 1 in France.
- Nausea, vomiting and diarrhea were the most commonly reported symptoms in COVID-19 patients. Nausea and vomiting were reported in 7% of the patients, while diarrhea in 6% of the patients. Other GI related symptoms include abdominal pain and anorexia.
- In terms of liver enzymes, elevated liver markers were observed in 16% of patients with non-severe infection and in 25% of patients with severe COVID disease. As compared to the general population, AST and ALT were increased by 20.54 U/L and 21.38 U/L in non-severe patients and 22.70 U/L and 22.94 U/L in severe patients, respectively, indicating elevation of liver enzyme in infected patients; however, with no significant difference between severe and non-severe infection.
- Other features observed in patients with severe disease include thrombocytopenia and hypoalbuminemia. In patients with severe infection, hypoalbuminemia was noticed in 90% of the cases, and 50% in non-severe COVID cases.
- In conclusion: This systematic-review and meta-analysis concluded that GI symptoms such as nausea, vomiting and diarrhea as well as elevated liver enzymes can be manifestations of COVID-19; therefore, we should have low index of suspicion for COVID infection in patients presenting with GI symptoms and absent of respiratory symptoms. Hypoalbuminemia and thrombocytopenia were found to be associated with severe infection.
Article PDF
Typhon Report
End of Rotation Self-reflection: Pediatrics
- How your perspective may have changed as a result of this rotation (e.g. elderly patients, kids, IV drug users, etc). During this rotation, I had the opportunity to rotate in different areas related to pediatrics including ER, neonatal ICU and clinics. Prior to this rotation, I saw pediatrics as one of the specialties of interest upon graduation. However, after getting exposed to NICU and pediatric primary care, it was enough for me to realize that pediatric is not a specialty I will see myself practicing. Assessing and managing pediatric patients can be challenging due to the huge variability in lab values, vitals, physical findings etc among the different age groups. Moreover, performing a physical exam as well as procedures (e.i IV, blood draws) can also be challenging especially if the child is inconsolable and crying. Adding to this, what it seems as a minor issue in the pediatric population can have a detrimental effect in their life and health if it is not identified or addressed promptly (e.i when kids don’t reach the expected developmental milestone or cranial sutures fused prematurely). This rotation certainly changed my perspective of the pediatric specialty.
- Exposure to new techniques or treatment strategies Respiratory complaints are very common in the pediatric population and therefore, it is very important to differentiate between upper and lower airway diseases. Related to these complaints, I learned a new and easy technique to assess lung sounds to differentiate upper and lower airway diseases by simply placing the stethoscope near the nose and then auscultating the lungs. If the adventitious sound is heard at nose and also in the lung fields, the pathology is likely due to an upper airway disease. This becomes relevant when ruling out/in upper airway diseases such as croup, epiglottis versus lower airway disease like asthma, pneumonia, bronchiolitis and bronchiectasis.
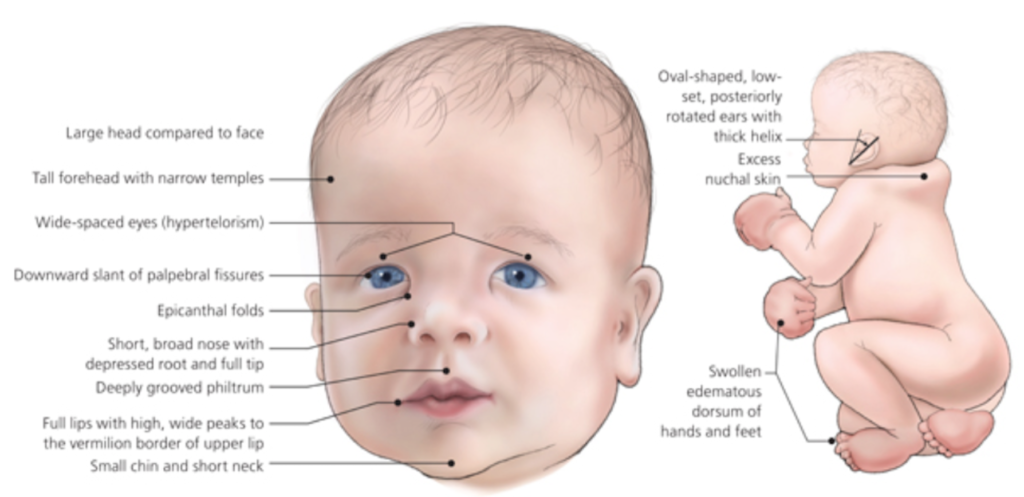
- What was a memorable patient or experience that I’ll carry with me? During my week in neonatal ICU, I examined a 2 week old newborn with a syndrome I never heard before. This newborn had a condition called Noonan syndrome, which is characterized by congenital heart disease, webbed neck, facial abnormalities, lymphedema, developmental delays, bleeding disorder, late onset of puberty, fertility issues, cryptorchidism, enlargement of liver and spleen, renal, eyes and skin problems. This newborn had a patent ductus arteriosus, wide space nipples, skin excess in the neck, umbilical and facial dysmorphia as well as low set ears and light eyes, which are other distinguishing features of Noonan. At birth, his extremities were swollen and his body was cyanotic. While examining this patient, I had the opportunity to listen to a patent ductus arteriosus for the first time. I will alway remember the characteristic features of Noonan syndrome due to this patient and of course how a patent ductus arteriosus sounds like.
Source:
Weismann, Constance, and Bruce D. Gelb. “Noonan Syndrome and Related Disorders.” Clinical Genomics: Practical Applications in Adult Patient Care, 1e
Evaluation Reflection
For my first site evaluation, I presented a 8 y/o male with a PMHx of biliary atresia (corrected a few months after birth) who presented to the ED with rectal bleeding x 4 days. This patient experienced 1-2 episodes of dark red bloody stools with clots as well as abdominal pain and recent symptoms of dizziness, headache, and nausea. Pt was previously seen at Mount Sinai for the same complaint, but was discharged with an unknown diagnosis. Abdominal ultrasound performed at Mount Sinai was significant for nonspecific parenchymal disease, splenomegaly and concerns for cirrhosis. During the ER visit, pt was given IV fluids and was transferred to Cohen’s Children Hospital for further work-up, which showed intense intestinal varices and portal hypertension; Pt will need a liver transplant. In our discussion, we touched about differential diagnosis for rectal bleeding in children. We also discussed the indications, monitoring and side effects of the drugs we encountered during our rotation.
For my second site evaluation, I presented a 17 y/o male without Pmhx who was brought to the ED by ambulance with complaints of epigastric pain and vomiting x 3 days. The epigastric pain started gradually two days prior to presentation and was described as dull, intermittent, non-radiating, and 10/10 without any alleviating or worsening factors. Pt also admitted feeling weak and having yellowish discoloration in eyes. Pt presented two days prior to the ED with the same complaint and was discharged with famotidine for gastritis. During ER visit, ALT and AST were found to be >7000 and >4, 781, respectively with pending hepatitis panel. Pt was transferred to Cohen’s Children Hospital. For this patient, there was no follow-up, but his hepatitis A came back as indeterminate. In our discussion with Prof. Maida, we were concerned that the patient’s liver enzymes were caused by other liver pathology and not due to viral hepatitis.