Daniela Arias Rodriguez
Emergency Medicine H&P #3 9 /7/20
Identifying Data:
Name: Mrs. L
Address: Queens, NY
Date of Birth: 55 yrs old
Date & Time: September 7, 2020
Location: NYPQ
Source of Information: Self
Source of Referral: self
Chief complaint:Lower abdominal pain x 1 month w/ bloody diarrhea.
HPI:Mrs. L is a 55 y/o Hispanic female with PMHx ulcerative colitis who presented to ED of NYPQ with complaints of diffuse abdominal pain x 1 month with multiple episodes of bloody diarrhea. Pain is crampy, intermittent, diffuse, more severe in the LLQ and 9/10 in severity. Pt reports that pain has gradually gotten worse since it started 1 month ago. She also reports 3-4 daily episodes of bloody diarrhea x 3 weeks as well as severe abdominal bloating right after eating. Pt is able to pass gases. Pt describes a mild similar episode in 2005 when she was diagnosed with ulcerative colitis. She denies taking any medication for ulcerative colitis. Pt denies nausea, vomiting, fever, fatigue, dizziness, weight loss, urinary symptoms, HA, chest pain, SOB, cough, sore throat, sick contact, new food, recent travel or COVID positive contact.
Past Medical History:
Present illnesses – ulcerative colitis
Past medical illnesses – gestational diabetes
Hospitalized – (see PSHx).
Immunizations -up to date
Colonoscopy- 2005, ulcerative colitis.
Past Surgical History:
C-section, unknown year
Medications:none
Allergies: No allergies
Family History:Non-contributory
Social History: Mrs. L is an Hispanic female who lives with her family. Pt denies smoking or use of alcohol and recreational drugs.
ROS:
Gen –Denies decrease in appetite, weight loss, fever, chills, fatigue or night sweats.
Skin, hair, nails—Denies dryness, excessive sweating, change in texture, dryness or change in hair distribution.
Head—Denies headache, vertigo, light-headedness or recent head trauma
Eyes—Denies blurring vision, photophobia, pruritus, dryness, diplopia, scotoma, lacrimation, fatigue with use of eyes or use of glasses.
Ears— Denies pain, discharge, hearing difficulty, use of hearing aids or tinnitus.
Nose/sinuses—Denies nose bleed, discharge or obstruction.
Mouth/throat—Denies sore throat/tongue, bleeding gums, mouth ulcers, changes in voice or use of denture.
Neck—Denies swelling, lumps, stiffness or decreased range of motion
Pulmonary – Denies dyspnea, cough, orthopnea, dyspnea, hemoptysis or wheezing.
CV—Denies chest pain, HTN, peripheral edema, palpitation, irregular beats, syncope and known heart murmur.
GI— report diffuse, intermittent and crampy abdominal pain x 1 month accompanied with daily episodes of bloody diarrhea x 3 weeks. Denies vomiting, nausea, decreased appetite, dysphagia, hematemesis, jaundice hemorrhoids or heartburn.
GU—Denies denies hematuria, frequency, nocturia, urgency, oliguria, dysuria, polyuria, hesitancy, incontinence or dribbling.
Menstrual/Obstetrical–LMP at age 51. G3P2012 nsd x2 and 1 sab. Denies being sexually active. Denies abnormal vaginal bleeding, discharge or itchiness. No abnormal previous pap smears.
Nervous— A&O x3. Denies hx of seizures, headache, loss of consciousness, numbness, tingling, ataxia, loss of strength and change in cognition or memory.
Musculoskeletal—Denies swelling, muscle pain, redness, deformity of muscles/ joints or arthritis.
Peripheral— Denies peripheral edema, coldness, intermittent claudication, varicose veins, and change in color.
Hematological— Denies easy bruising, anemia, hx of blood transfusion, lymph node enlargement or Hx of DVT/PE.
Endocrine—Denies polyuria, diaphoresis, polydipsia, polyphagia, heat or cold intolerance, goiter and hirsutism.
Psychiatric— Patient denies depression or suicidal ideations.
VS:T 36.8 C orally, HR 80 bpm, BP 92/54 Right arm lying in bed, RR 20, SpO2 98% room air, BMI: 20.5
Physical Exam:
Gen– AOx3, in apparent distress, average build and appears her stated age.
Skin: warm & moist, good turgor, non-icteric, no visible lesions, scars or tattoo.
Nails: no signs of clubbing, lesions, paronychia, capillary refill <2 second.
Hair: Evenly distributed with no signs of erythema or dryness in the scalp.
Head:Normocephalic, non-tender to palpation with no signs of swelling or trauma.
Ear: Intact tympanic membrane with undisturbed cone of light bilaterally. No lesions or erythema in the auditory canal bilaterally. Whispering test unremarkable bilaterally.
Eyes:white sclera and pink conjunctiva bilaterally. PERRLA, full visual fields and intact EOM with no nystagmus. Visual acuity 20/20 bilaterally. Unremarkable optic disc, no hemorrhage or exudates bilaterally on fundoscopy.
Mouth: pink and moist mucosa with no masses, thrush or lesions. No signs of tonsil exudate or enlargement. Uvula middle line with no signs of edema or lesion.
Trachea/thyroid:midline and non-tender to palpation. Non-palpable nodule or bruit on auscultation. No lymphadenopathy.
Lungs: Clear to auscultation bilaterally. No rales, rhonchi or wheezing on auscultation. No signs of labored breathing. Unremarkable egophony and tactile fremitus.
Cardiac:Normal S1/S2 and RRR. No murmur, JVD or carotid bruits noticed.
Abdomen:Markedly distended abdomen with 8 inch c-section scar. Bowel sound present in all 4 quadrants. Tenderness to palpation in all quadrants. No guarding, rebound tenderness or sign of ascites. Negative Murphy’s sign, psoas, obturator tests and CVA tenderness.
GU: No masses or lesions on vulva or vaginal introitus. No signs of inflammation, discharge or erythema on vaginal mucosa or cervix. No cervical motion tenderness. Small and mobile uterus. Adnexa without masses or tenderness.
Rectal:. No lesions, fissures, hemorrhoids or stool in rectal vault. Good sphincter tone. Negative guaiac.
Extremities: Full passive and active ROM in upper and lower extremities bilaterally. 2+ pulses in upper and lower extremities. No sign of edema,muscle atrophy or muscle atrophy.
Neurology: A&O x 3. Intact finger to nose test. Intact rapid alternating movement and heel-to-shin test. Intact sensation in UE and LE bilaterally. Muscle strength 5/5 in UE and LE. Cranial intact 2-12. Unremarkable gait and negative Romberg test. No signs of asterixis. Biceps, patellar and ankles reflexes 2+ bilaterally.
DDX
- Ulcerative colitis flare-up
- Small bowel obstruction
- Large bowel obstruction
- Diverticulitis
- Hemorrhoids
Assessment/plan: Mrs. L is a 55 y/o Hispanic female with PMHx of Ulcerative colitis presented to the ED of NYQP with diffuse abdominal pain x 1 month with multiple episodes of bloody diarrhea. CT abdomen revealed wall thickening involving the transverse and sigmoid colon compatible with ulcerative colitis. Abdominal exam was significant for distended abdomen and tenderness to palpation in all quadrants.
- Give IV fluids and recheck blood pressure. BP 92/54 at triage.
- Give 15 mg Toradol IV for pain
- Zofran 4mg as needed.
- Discharge with 4g enema PR at bedtime of Mesalamine for 3-6 wks and 800 mg PO tid x 6wks of oral Mesalamine.
- Recheck CBC and blood pressure before discharge. (Hct: 30.4, Hgb: 10.0)
- Give GI referral to establish maintenance therapy for ulcerative colitis.
Article Summary
Chandan S, Mohan BP, Chandan OC, Ahmad R, Challa A, Tummala H, Singh S, Dhawan P, Ponnada S, Singh AB, Adler DG. Ann Gastroenterol. 2020 Jan-Feb;33(1):53-58. doi: 10.20524/aog.2019.0439. Epub 2019 Nov 29.PMID: 31892798
-
Although this journal is not currently indexed by Medline, it is systematic review and meta-analysis published in 2020.
-
It included seven RCTs with a total sample size of 380 patients with ulcerative colitis. 188 patients were treated with curcumin and mesalamine and 192 patients were given placebo with mesalamine. Of the 380 patients, 174 were males and 128 were females with a mean age range from 32.7 (+/- 8.9 yrs) to 45.2 (+/- 15.8 yrs).
-
Six studies used oral curcumin, while one study used rectal curcumin. Lowest curcumin dose used was 100mg and maximum dose used was 1000mg.
-
As per Jadad scale, all studies were graded as having high quality.
-
Treatment response was measured by using several indices such as Clinical Activity Index (CAI), Simple Clinical Colitis Index (SCCAI) and Disease Activity Index (DAI)
-
Outcomes assessed include pooled rate of clinical remission, pooled rate of clinical response, pooled rate of endoscopic response and remission and safety profile.
Results:
-
Pooled odd ratio for clinical remission with curcumin was 2.9 (p=0.002)
-
Pooled rate of clinical response was 2.6 (p=0.001)
-
Pooled odd ratio for endoscopic response and remission was 2.3 (p=0.01)
-
In terms of safety profile, one study reported 3 serious adverse effects that caused the withdrawal of participants from the study. Four participants reported mild adverse effects such as nausea, increased stool frequency and abdominal bloating.
Conclusion: This meta-analysis and systematic review concluded that use of curcumin in conjunction with mesalamine provides better clinical and endoscopic treatment response for ulcerative colitis as compared to mesalamine alone. This study recommended its use as an adjective treatment given its minimal side effects
Article PDF AnnGastroenterol-33-53
Evaluation Reflection In the first site evaluation, I presented a 88 y/o Hispanic male with PMHx of colon cancer (treated 2yrs ago), HTN and BPH who was referred to ED by his PCP due to elevated LFTs and yellowish skin. Physical exam was pretty much unremarkable, except for an icteric sclera and severe jaundice. Pt came to ER 15 days ago with complaints of hematuria and was discharged with antibiotics for positive UTI. Abdominal CT was significant for pancreatic adenocarcinoma in the head/neck of the pancreas with possible extension to the duodenum and metastasis to the liver. Patient was admitted to the medicine floor. When I presented this patient to Prof. Mohamed, he was very skeptical for the fact that this patient came to ER 15 days prior and no elevation of transaminases were noted. This case was very shocking to me, since I got to build some rapport with the patient while he was in the ER. I was frequently checking on him during the shift, so communicating the bad would have been a little bit challenging for me.
For the second site evaluation, I presented a 55 y/o Hispanic female with PMHx ulcerative colitis who presented to ED with complaints of diffuse abdominal pain x 1 month with several episodes of bloody diarrhea. A CT of the abdomen confirmed an ulcerative colitis flare-up. The patient was given pain medication, augmentin and discharged home. In our discussion with Prof. Mohamed, he suggested that the appropriate management would have been admitting this patient to hospital. He highlighted the importance of monitoring more closely hemoglobin and hematocrit in these patients due to the bloody diarrhea. This is something I will certainly keep in mind when treating ulcerative colitis patients. In the final evaluation, he suggested that I should be more detailed in my plans. I knew that I needed improvement in this area, and I will certainly keep it in mind to improve it.
End of Rotation Self-reflection: RT
- What did you learn about yourself during this 5-week rotation? Emergency Medicine was the rotation I was waiting for to decide what specialty I want to do. Initially, I was debating between internal and emergency medicine, and I found out that I LOVE emergency medicine. In emergency medicine, you get instant gratification by seeing your patient doing better or providing instant relief. As compared to internal medicine, in the ER there is more hand-on experience with the patients such as doing laceration repair, needle decompression, diagnostic ultrasounds, splinting, wound care, intubation, etc. I also love emergency medicine, because we rely heavily on the physical exam findings and history to guide testing and diagnosis. Sadly, during my internal medicine rotation some practitioners barely performed physical assessments on their patients. Of course, everyone practices medicine differently! At first I was concerned about working under high pressure like it happens in the ER; however, I discovered that I can handle it more than I expected. During this rotation, it was very reassuring to get certain critical diagnoses right, and these were diagnoses that I was suspecting. Love the adrenaline of ER, and I’m certainly looking forward to working in this field.
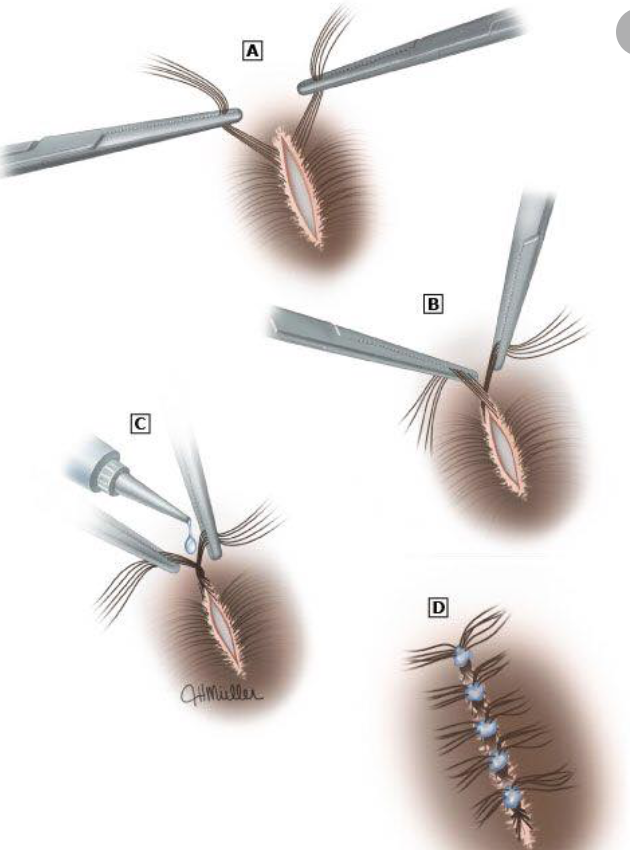
Exposure to new techniques or treatment strategies – how did that go? During this rotation I had the opportunity to do the hair apposition technique for a laceration repair. I performed this technique on a patient who fell backward while going upstairs. The patient got two 3cm lacerations on the scalp. In this technique, hair from both sides of the laceration is twisted to create a node at the center of the laceration to approximate the edges. After the node is in place, dermabond (surgical glue) is used to secure it. This technique can be used for minor scalp lacerations that are not too deep. In this patient, the physician assistant did a demonstration first and then I took over. To be the first time, It went very well

Skills or situations that are difficult for you (e.g. presentations, focused H&Ps, performing specific types of procedures or specialized interview/pt. education situations) and how you can get better at them. As I mentioned in my previous reflexions, IV placement and blood draws were skills that I wanted to improve. During this rotation, I had the opportunity to do these procedures. I certainly feel more confident now when doing blood draws, but I still need to improve IV placement. As I was told, the best strategy to get better at doing IV placement is by practicing. I hope to keep working on this skill during my surgery or pediatric rotation.
Typhon Report

