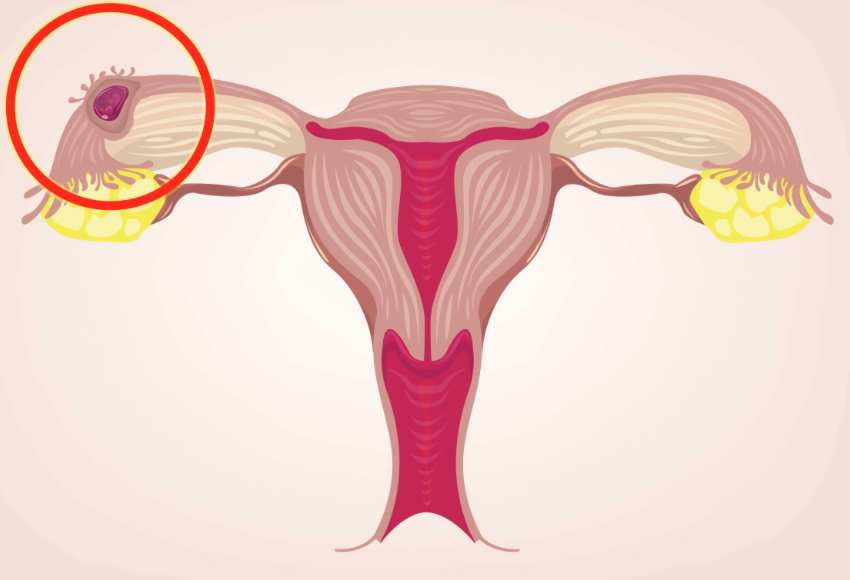
Treatment of Ectopic Pregnancy
Ectopic pregnancy can be managed in three different ways: surgery (salpingostomy or salpingectomy), methotrexate and expectant management. When an early diagnosis is performed, most patients are treated with methotrexate.
In which situations is methotrexate therapy preferred over surgery?
- If the patient is hemodynamically stable
- If the serum beta hCG is less or equal to 5000 mU/ml
- If there is not fetal cardiac activity or the ectopic mass is < 3-4 cm. However, a mass of 3.5 cm or greater is a contraindication to give MTX.
- If patients agree to follow-up posttreatment and have accessible emergent medical services in case of rupture.
Methotrexate and surgery are considered equally effective. Although, multiple or single doses of MTX can be administered depending on multiple factors. Patients with high hCG concentration >5000 mU/ml are more likely to require multiple doses of MTX. High level of serum hCG is the most significant indicator of MTX treatment failure. Evidence of yolk sac, ectopic mass located at the isthmus, high level of folic acid, and increase/or fall in hCG before or within a few days after starting treatment are other indicators of MTX treatment failure.
In which situations is surgery indicated and methotrexate contraindicated?
- If patient is hemodynamically unstable (like our patient)
- If there is a viable intrauterine pregnancy as well as an ectopic pregnancy
- Signs and symptoms indicating rupture of ectopic mass such as pelvic or abdominal pain or findings indicating intraperitoneal bleeding. US findings consistent with peritoneal fluid is a criteria that exclude MTX as treatment.
- Patients with baseline abnormalities in hematologic, renal and hepatic labs values (in patients with renal insufficiency, a single dose of MTX can cause bone marrow suppression, ARDS, bowel ischemia, or death) (In patients with renal and liver dysfunctions, MTX can lead to pancytopenia and skin/mucosal disorders due slow metabolism of MTX)
- If patient is breastfeeding
- If the patient has certain medical conditions such as immunodeficiency, current lung diseases, and peptic ulcer disease.
- If the patient has hypersensitivity to MTX.
When it comes to surgery, there are two surgical methods, salpingectomy (removal of fallopian tubes) and salpingostomy (removal of affected tube and leaving the remainder intact). Salpingectomy is considered the standard procedure; however, salpingostomy is preferred for being a conservative surgery. In patients that are hemodynamically stable, surgery should only be performed if the transvaginal US shows a tubal ectopic pregnancy or adnexal mass indicating ectopic pregnancy. If the mass cannot be identified in the TVUS, it might be very difficult to palpate or identify the mass during surgery. Women can choose surgery if they prefer a treatment of short duration, requiring less follow-up, and agree with the risk and cost of recovery associated with surgery. Surgery can be an option for women who are considering definitive sterilization methods.
Expectant management is considered for a very small number of patients with an ectopic pregnancy with whose location is unknown and have low risk of fallopian tube rupture. Expectant management might be considered in women with US findings not showing gestational sac outside of uterus or extrauterine mass indicating ectopic pregnancy. Women with beta hCG <200 mU/ml and declining can be considered for expectant management as well for women willing to comply with follow-up and accessible emergent medical services.
Sources
- https://www-uptodate-com.york.ezproxy.cuny.edu/contents/ectopic-pregnancy-choosing-a-treatment?search=ectopic%20pregnancy%20treatment&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1
Stages of Labor Labor is divided into three stages. The first stage starts with the onset of labor and concludes with the full dilation of the cervix. The first stage is further divided into latent and active phases. The second stage is the period between complete cervix dilation to the delivery of the infant. The third stage starts with the delivery of the infant and ends with the delivery of the placenta.
Labor is divided into three stages. The first stage starts with the onset of labor and concludes with the full dilation of the cervix. The first stage is further divided into latent and active phases. The second stage is the period between complete cervix dilation to the delivery of the infant. The third stage starts with the delivery of the infant and ends with the delivery of the placenta.
First Stage of labor. As mentioned previously, the first stage starts with the onset of labor and ends with the full dilation of the cervix. The latent phase is marked with the onset of labor and initiation of active labor. During this phase, the cervix undergoes effacement and dilation. In this phase, the cervical changes are slower with the contractions. However, in the active phase, the cervix goes through more rapid changes. The start of the active phase is noticed with a cervix dilation of at least 6 cm with cervical changes of 0.5-0.7 cm/ hr in nulliparous and 0.5-1.3 cm/ hr in multiparous women. Active phase arrest is considered in women a dilation of >6cm with rupture of membrane who fail to progress dilation for 4hrs despite adequate contractions or administration of oxytocin for at least 6 hours.
Fetus can be monitored intermittently by auscultation or electronic fetal heart tracing at least every 30 minutes in the active phase and the second stage of labor every 15 minutes. If the mother has complications, the fetus should be monitored continuously. Uterine contractions can be monitored by palpation, tocodynamometer or internal pressure catheter. If monitored by palpation, frequency, duration and intensity should be palpated every 30 minutes. In the latent phase cervical examination is minimal, but in the active phase cervix dilation should be assessed every 2 hours to monitor progression of labor.
Second Stage of Labor is the period between complete cervix dilation to the delivery of the infant. During this stage, the mother feels the need to bear down with each contraction. To monitor progression of labor, the descent of the fetal head is measured. This is done by determining the position of fetal head in relation to the maternal ischial spines. If the fetal head is at the level of ischial spines, the station (estimates the numbers of cm from the ischial spine) is zero. If the fetal head above the ischial spines, the station is -2 and if it is below ischial spines is +2. The second stage can have a duration of 30 minutes to 3 hrs in primigravid and 5-30 minutes in multigravida females. When crowning occurs (fetal scalp is visible at the introitus), the fetal head should be controlled to reduce risk of laceration. Basically, you want to apply counter pressure to prevent any laceration to the mother peritoneum. After the head is delivered, the baby nose should be suctioned and the neck should be evaluated for nuchal cord. For the shoulders, apply downward traction to deliver the anterior shoulder and upward traction to deliver the posterior shoulder. After the body is delivered, clamp and cut the umbilical cord. Delayed cord clamping (30-60 sec) can cause high levels of hemoglobin and increased iron stores in the first several months of life.
Third Stage of Labor starts with the delivery of the infant and ends with the delivery of the placenta. After delivery of the baby, the cervix, vagina and perineum should be inspected for laceration causing active bleeding and possible surgical repair. The placenta usually detaches in 30 minutes. You want to observe signs indicating placental separation such as lengthening of the umbilical cord, fresh blood at the vagina, rise of fundus superiorly and firm/globular uterus. After delivery of the placenta, it should be inspected for abnormalities and integrity along with the cord and membranes.
The puerperium is the period following the delivery of the baby and placenta until 6 weeks postpartum. An hour after delivery, the mother’s blood pressure, heart rate and blood loss from the uterus must be monitored. During this time, hemorrhages caused by unrepaired laceration, relaxation of the uterus and retained membranes or placenta fragments are likely to occur. This time is important for maternal and newborn bonding and initiation of breastfeeding.
Sources
- Bennett, Terri-Ann, et al.. “Normal & Abnormal Labor & Delivery.” CURRENT Diagnosis & Treatment: Obstetrics & Gynecology, 12e Alan H. DeCherney, et al.New York, NY: McGraw-Hill, , http://accessmedicine.mhmedical.com.york.ezproxy.cuny.edu/content.aspx?bookid=2559§ionid=207399535.
- OB/GYN class. Intrapartum care slides.
D-dimer and Pregnancy
What is D-dimer?Is the main degradation product of fibrin. It is produced by the cleavage of crosslinked fibrin by plasmin. In the process, plasmin also generates other fibrin degradation products (FDPs); however, D-dimer has the most clinical value. Normal plasma levels of D-dimer are 500ng/ml by ELISA testing or 250 ng/ml for D-dimer units. High level of D-dimer indicates recent or active coagulation and breakdown of fibrin in the vasculatures.
What happens to D-dimer during pregnancy?
D-dimer has a high negative predictive value in nonpregnant patients, and therefore can be used to exclude DVT. However, in pregnant patients, D- dimer is elevated and despite its high negative predictive value it is not as useful for diagnosis. D-dimer naturally rises during each trimester and declines after delivery or postpartum explaining its limited use. There is not an established normal range before and after delivery of D-dimer due to limited studies. In a study of 50 pregnant females without venous thrombosis, it was found that D-dimer increased with each subsequent trimester. In the second trimester, 22 % were found to have a normal D-dimer, but in the third trimester none of the females had a normal D-dimer.
What other conditions can increase D-dimer?
- DVT
- Pulmonary embolism
- Atrial fibrillation
- Myocardial infarction
- Strokes
- DIC
- Preeclampsia and eclampsia
- Surgery, trauma
- Renal disease
- Severe infections
- Vaso-occlusive episode of sickle cell
Sources:
- https://www-uptodate-com.york.ezproxy.cuny.edu/contents/deep-vein-thrombosis-in-pregnancy-epidemiology-pathogenesis-and-diagnosis?search=d%20dimer%20in%20pregnancy&source=search_result&selectedTitle=3~150&usage_type=default&display_rank=3#H1323764
- https://www-uptodate-com.york.ezproxy.cuny.edu/contents/clinical-use-of-coagulation-tests?search=d%20dimer&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1#H92754657
Effect of the combined oral contraceptive pill and/or metformin in the management of polycystic ovary syndrome: A systematic review with meta‐analyses. Helena Teede1,2 | Eliza C. Tassone1 | Terhi Piltonen3| Jaideep Malhotra4|Ben W. Mol5| Alexia Peña6| Selma F. Witchel7| Anju Joham1,2| Veryan McAllister8|Daniela Romualdi9 | Mala Thondan,10| Michael Costello11| Marie L. Misso1
- This is a systematic review with meta-analysis of randomized control trials published in 2019. This article is also indexed by Medline. This systematic review and meta-analysis aimed to answer how effective is oral contraceptive pill and metformin alone or combined at managing the clinical, weight and hormonal imbalances in adolescents and adults with polycystic ovarian syndrome (PCOS).
- Electronic databases were searched on January 11, 2017. A total of 3205 studies were obtained of which 56 studies met the inclusion criteria.
- The search was restricted to systematic-reviews published in english language, randomized control trial and without restrictions to publication year. Crossover studies were included as long as a washout period was performed for more than 8 weeks.
- For this systematic-review and meta-analysis, the population of interest was female with diagnosed PCOS of any ethnicity, weight and age. Target interventions included contraceptive pills alone or in combination with metformin, life-style, antiandrogens or antiobesity agents as well as metformin alone or combined with OCPs, lifestyle, antiandrogens, antiobesity agents and placebo.
- Most of the included studies had a duration treatment of 3 months and 24 months. The sample size across the studies ranged from 10 to 253 participants. In terms of age groups, six studies were done in adolescents, forty-eight in adults and two did not specify age groups. Across the studies, the average BMI ranged from 18.50-24.99 kg/m2 to obese participants with BMI >40 kg/m2.
- The included studies were determined to have low, moderate and high risk of bias.
- This systematic review and meta-analysis concluded that combined oral contraceptive pills improve hyperandrogenism and irregular menstrual cycles in adults and adolescent women with polycystic ovarian syndrome (PCOS). It ratified the effectiveness of metformin alone or in combination with COCP at treating the metabolic, weight and hormonal imbalances seen in PCOS particularly in women with BMI >25 kg/m2. These researchers recommended metformin for prevention of weight gain and improvement in hormonal and metabolic outcomes like testosterone, cholesterol and triglyceride. Mild gastrointestinal symptoms were noticed with the addition of metformin to COCP, which may affect medication compliance.
Sources:
- https://www.ncbi.nlm.nih.gov/pubmed/31087796